Reports
Reports

Tired of CME doctor’s discrediting your
clients’ injuries?
Have a licensed doctor review your CME video and report exposing any issues in the exam. Too many times CME doctor’s report negative testing or perform orthopedic tests incorrectly without you knowing. Below is an example of what to expect after we review your CME file. We give you key questions and info to ask the CME Dr at deposition.

references

Intro
History and exam with patient was approximately a 14 minute 30 second encounter.
History questions and dictation was approximately 12 minutes.
Cranial Nerve Exam 2-12 was approximately 15 seconds.
Low Back exam was approximately 1 minute 15 seconds.
Neck exam was approximately 1 minute.
Here is a recent example for one of our reports
How did you perform a sensory exam of upper and lower extremities to rule out or determine a radicular dermatomal pattern from the cervical or lumbar spine?
how did you perform a straight leg raise?
- At 12:30-12:45, the patient clearly does NOT have full range of motion in all planes of motion. Especially on left rotation.
- According to NIH, cervical Spine ROM is approximately 80-90 degrees of flexion, 70 degrees extension and 90 degrees of rotation. (6)
- Inclinometer’s and/or goniometers allow a consistent and standardized method in evaluation of rom providing objective data in degrees. Why were these not used?
- Once again Dr does no objective testing to back up his opinion that Mrs. Martin was not injured by this crash on 10/13/21.
What ortho tests did you perform to determine or rule out any radicular symptoms from disc involvement in her neck?
“On page 2 of Dr’s report he states that he reviewed all patients MRI’s. He states “In my opinion, there is simply nothing on those scans which should be a source of pain.”
Intro
History and exam with patient was approximately a 14 minute 30 second encounter.
History questions and dictation was approximately 12 minutes.
Cranial Nerve Exam 2-12 was approximately 15 seconds.
Low Back exam was approximately 1 minute 15 seconds.
Neck exam was approximately 1 minute.
Questions:
1.) Did you fully test cranial nerves 2 through 12 for any abnormalities?
Approximately how long does a full cranial nerve exam take testing nerves 2-12?
- Dr starts his cranial nerve testing at 10:45-11:00. A total of 15 seconds.
- Dr has patient look left, right, up and down testing cranial nerves 3,4 and 6.
- Dr makes a noise in both ears asking if she hears it testing cranial nerve 8.
- Dr asks patient to shrug her shoulders up testing for cranial nerve 11 the accessory nerve. (Not done correctly.)
- He did NOT test Cranial nerve 2, 5, 7, 9+10, 11 properly or 12 (details below)
- He states on page 2 “Cranial nerves 2 through 12 appear to be intact”. How can you come to that conclusion without testing all them?
- There are 12 cranial nerves that should be tested with multiple tests associated with each. Dr did the test starting at 10:45-11:00. A little over 15 seconds to test 12 cranial nerves accurately is not possible. I have attached Merck Manual video on each test in reference page. (1 +2)
- Cranial Nerve 1 Olfactory Nerve. This test is performed covering each nostril and testing ability to smell seeing if the olfactory nerve is intact. This was NOT tested. In his report though he doesn’t state he tested it.
- Cranial Nerve 2, Optic Nerve. The doctor only tested visual fields, only one component of the testing. NO visual Snell eye chart was used. NO pen light was used to check eye pupil constriction.
- Cranial Nerve 3,4,6 was done adequately.
- Cranial Nerve 5, Trigeminal Nerve. Light touch sensation of Vl (Ophthalmic), V2 (Maxillary) and V3 (Mandibular) regions were NOT tested. Cotton swabs should have been used to test each region left and right side of specific nerve dermatomes of the face. The muscles temporalis, masseter and Pterygoids should then have been tested for overall strength. None of those muscles were tested.
- Cranial Nerve 7, Facial Nerve. This nerve was NOT tested properly if at all. Tests strength of facial muscles. Dr should have had patient first raise eyebrows to check those muscles. Dr. then should have instructed the patient to close her eyes while he tried to pull them open lightly. Last, he should have had her smile showing teeth to look for any asymmetry from side to side.
- Cranial Nerve 8, Vestibulocochlear Nerve. This was tested correctly.
- Cranial nerve 9+10, glossopharyngeal nerve and Vagus nerve. Dr did NOT check these nerves. These are nerves that control the mouth and soft palate. Dr should have had patient open her mouth looking for soft palate or uvula deviation. Next Dr should have had patient make the sound E or Ah.
- Cranial nerve 11, Accessory Nerve. This test was NOT performed correctly. This tests the motor strength of the Trapezius and Sternocleidomastoid muscles. Patient should have shrugged shoulders up while DR actively resisted down to test trapezius strength. Next Dr should have had patient try to turn their head into his resisting hand, testing strength of sternocleidomastoid.
- Cranial Nerve 12, Hypoglossal Nerve. This was NOT tested. This cranial nerve controls the muscles of the tongue. Dr should have had patient stick tongue out looking for deviations and testing for strength.
2.) How did you perform a sensory exam of upper and lower extremities to rule out or determine a radicular dermatomal pattern from the cervical or lumbar spine?
- Page 2 of his report patient tells Dr that “sometimes all her fingers go numb.” Dermatomes must be adequately tested.
- No sensory testing was performed.
- When performed according to criteria in the AMA Guides to the Evaluation of Permanent Impairment (AMA Guides), Fourth Edition, upper and lower extremity impairment assessment requires a thorough physical examination of the involved (and contralateral) limb. According to the AMA Guides, sensory testing, requires equipment and considers all sensory modalities, including perception of pain, heat, cold, and touch. For example, the two-point discrimination test of sensory quality can be performed using a paper clip or commercially available test disks. Traditionally, light touch is assessed using a cotton tipped swab, and sharp-dull discrimination can be assessed using a safety pin or needle (discard after use). Pressure and vibration sensibility can be assessed using the end of an initially still, then vibrating 128-Hz tuning fork. (3)
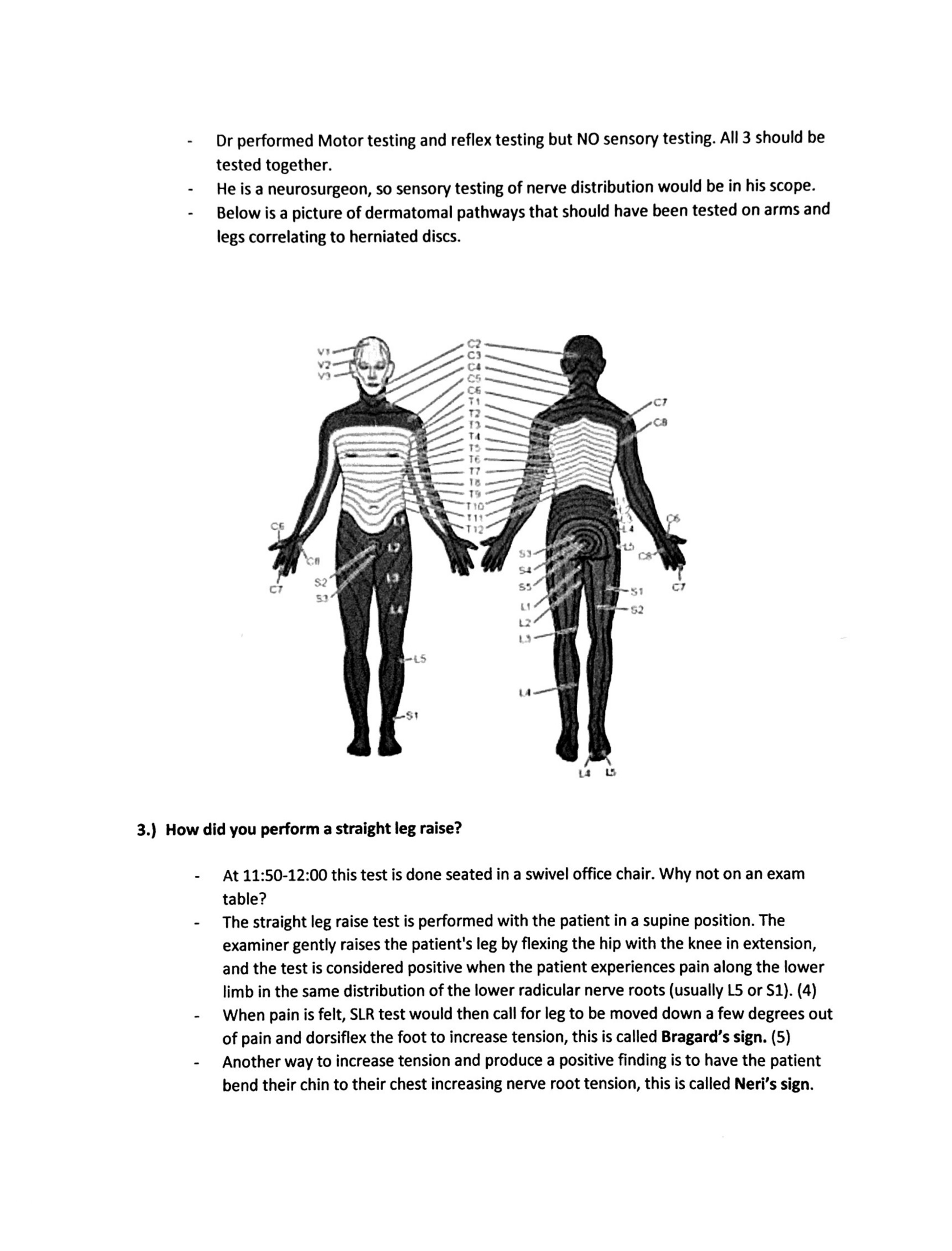
- Dr performed Motor testing and reflex testing but NO sensory testing. All 3 should be tested together.
- He is a neurosurgeon, so sensory testing of nerve distribution would be in his scope.
- Below is a picture of dermatomal pathways that should have been tested on arms and legs correlating to herniated discs.

3.) How did you perform a straight leg raise?
- At 11:50-12:00 this test is done seated in a swivel office chair. Why not on an exam table?
- The straight leg raise test is performed with the patient in a supine position. The examiner gently raises the patient’s leg by flexing the hip with the knee in extension, and the test is considered positive when the patient experiences pain along the lower limb in the same distribution of the lower radicular nerve roots (usually LS or S1). (4)
- When pain is felt, SLR test would then call for leg to be moved down a few degrees out of pain and dorsiflex the foot to increase tension, this is called Bragard’s sign. (5)
- Another way to increase tension and produce a positive finding is to have the patient bend their chin to their chest increasing nerve root tension, this is called Neri’s sign.
- The whole idea of these tests is to reproduce the pain by forcing joints to end range. Dr is not trying to provoke the pain the way he is performing these tests, nor did he perform it correctly.
- Dr. never even asks Mrs. Martin if she Is beginning to feel any pain. But on page 3 of report states straight leg raising test is negative bilaterally.
4.) How did you determine patient’s neck had ”good range of motion” on page 3 of your report?
- At 12:30-12:45, the patient clearly does NOT have full range of motion in all planes of motion. Especially on left rotation.
- According to NIH, cervical Spine ROM is approximately 80-90 degrees of flexion, 70 degrees extension and 90 degrees of rotation. (6)
- Inclinometer’s and/or goniometers allow a consistent and standardized method in evaluation of rom providing objective data in degrees. Why were these not used?
- Once again Dr does no objective testing to back up his opinion that Mrs. Martin was not injured by this crash on 10/13/21.
5.) What ortho tests did you perform to determine or rule out any radicular symptoms from disc involvement in her neck?
- Zero orthopedic tests performed on the neck. Most sensitive test for this would be Spurling’s.
- Spurling test is designed to provoke radicular symptoms in the neck by reducing the diameter of the IVF (Intervertebral foreman).
- Most provocative position producing distal pain is Extension, Lateral Bending with Axial compression. (7)
- Dr may say that he is a neurosurgeon, and this type of orthopedic testing is out of his scope of practice. Issue is why did he then do a straight leg raise that looks for disc involvement in the lower back?
6.) On page 2 of Dr’s report he states that he reviewed all patients MRI’s He states “In my opinion, there is simply nothing on those scans which should be a source of pain.”
- Dr reviewed lumbar and cervical MRI’s I don’t have access to those images or reports but at 10:14 Dr asks patient do you know why you are having this pain? She responds “Dr. Torres says because I have herniated and bulging discs in my neck and back.”
- So you are saying that it is impossible for multiple disc bulges and herniations (confirmed on imaging) to produce any pain in a person? There is zero correlation between the two?
- According to Mayo clinic (where it says on his website he was trained) (8) that compared with a bulging disk, a herniated disk is more likely to cause pain because it generally protrudes farther and is more likely to irritate nerve roots.(9)
Conclusion/ Closing Thoughts:
- Extremely brief exam of neck and back.
- 15 second cranial nerve testing.
- Did not test all cranial nerves that he said were intact.
- Zero sensory testing of upper and lower extremities.
- No ortho neck testing.
Call or email me with any questions.